2Department of Radiation Oncology and Medical Physics, Jawaharlal Nehru Cancer Hospital and Research Centre, Bhopal-India DOI : 10.5505/tjo.2022.3657
Summary
OBJECTIVEIn this study, we analyzed dose to organ at risk in the left breast cancer patients, in terms of dose volume histogram (DVH), with the quantitative analysis of normal tissue effects in the clinic dose constraints and calculate potential toxicity in terms of normal tissue complication probability (NTCP).
METHODS
This study included 60 post-operated left breast cancer patients who received chest wall/breast irradiation
by three-dimensional conformal radiotherapy (RT). The patients had received a total dose of 40Gy
in 15 fractions to whole breast/chest wall (two fields) and dose to supraclavicular fossa (three fields). We
compared the DVH for heart, lung, and spinal cord in both fields.
RESULTS
Mean dose for lung was 17.49Gy and for heart 12.31Gy, and spinal cord maximum dose was 0.78Gy.
The average lung NTCP for RP was 3.11%. The risk of RP was significantly greater in three-field radiation
as compared to two field for lung (p<0.05). We observed the statistically significant correlation
of MHD and NTCP (p<0.00001 and p=0.000402). The correlation of central lung distance (CLD) was
observed to be significant with three fields, that is, as the CLD increased risk of organ damage to lungs
increased (p=0.00022). The correlation of CLD and MHD with DVH was observed to be statistically
significant (p<0.001).
CONCLUSION
This study results are useful to reanalyze the previous 2D-based clinical reports about breast RT complications
as a view point of the NTCP. Further studies are needed for the actual clinical data of complications
with this DVH analysis.
Introduction
Breast cancer is the second most common malignancy in the world. In India, breast cancer is the most common cancer diagnosed, with 200,000 (14.8%) of the total cancer cases according to the Indian Council of Medical Research.[1] Whole breast radiotherapy (RT) after lumpectomy and chest wall post mastectomy RT (PMRT) both have shown improved locoregional control and definite survival benefit.[2,3]There have been concerns regarding an increase in cardiac mortality, especially in patients who had been treated with RT for the left-sided breast cancer.[4-6] This latent manifestation of cardiovascular disease is of great importance, since the survival rate for breast cancer patients is improving and breast cancer patients have remarkable life expectancy after completing treatment.[7-10]
As recommended by normal tissue complication probability (NTCP) models for cardiac mortality, it should be considered that NTCP value more than 5% could jeopardize the beneficial effect on survival of RT.[11] The NTCP of cardiac mortality increased with maximal heart distance (MHD), and the NTCP of radiation-induced pneumonitis (RP) increased with central lung distance (CLD).[12]
Thus, the purpose of this study is the dosimetric analysis of organs at risk (OAR) in the left breast cancer patients, in terms of dose volume histogram (DVH) to analyze adherence of plan with the quantitative analysis of normal tissue effects in the clinic (QUANTEC) dose constraints and calculate potential toxicity in terms of NTCP.
Methods
Study DesignThis prospective analytical study was initiated and followed by approval from the Institutional Ethical Committee. A written informed consent has been obtained from every patient enrolled in this study. From January 2018 to March 2019, a total of 60 post-operated (breast conservation surgery or mastectomy) patients of histopathologically proven left breast carcinoma who received chest wall/breast irradiation by three-dimensional conformal RT (3D-CRT) technique at a RT Center of Central India were enrolled in this study. The patients included in the study had stage I to III breast cancer, underwent post modified radical mastectomy or post breast conservation surgery, were between 18 and 70 years of age, had Karnofsky Performance Score more than 70, had received a total dose of 40 Gy in 15 fractions to whole breast/chest wall, and those who received 40 Gy in 15 fractions to supraclavicular fossa (SCF) or 10-12 Gy electron beam boost to tumor cavity. The patients who were excluded from the study were <18 or more than 70 years of age, had metastatic disease (stage IV), and had received irradiation by use of accelerated partial breast irradiation, interstitial implants, intraoperative RT or intensity modulated RT, and those with uncontrolled cardiovascular or renal medical conditions.
Patient positioning and fixation
Patients were positioned in the supine position, on an
angled board such that the sternum was horizontal
with the ipsilateral arm abducted to 90°. The patient
must remain in identical position for computed tomography
(CT) simulation and subsequent treatment.
Patients were immobilized using thermoplastic mold.
Care must be taken at data acquisition to adapt all the
supporting devices to the individual patient"s size and
shape to maximize comfort, and so aid reproducibility
for subsequent treatment.
Clinical landmarks
The target was defined to consist of the chest wall/
breast and SCF. The chest wall/breast borders consisted
of the medial border at or 1 cm over the patient"s
midline, the lateral border at 2?3 cm beyond
all palpable breast tissue to the mid axillary line, the
superior border at the sternal angle, and the inferior
border at 2 cm below the contra lateral inframammary
fold. SCF borders are delineated as the superior
border at thyrocricoid groove, the inferior border
matched with upper border of tangential field, the
medial border at or 1 cm across midline extending
upward following medial border of sternocleidomastoid
muscle to thyrocricoid groove, and the lateral
border at insertion of deltoid.
Data transfer methods and algorithm
Three-dimensional CT imaging scans multiple slices
with slice thickness 5 mm were obtained with the patient
in the treatment position that was used throughout
treatment. A reference point was defined and
marked on the customized thermoplastic mold used
for patient immobilization.
CT cuts were transferred in the digital imaging and communications in medicine (DICOM) format images and viewed using treatment planning system (TPS) Eclipse version 15.6 (Varian Medical Systems, Palo Alto, CA, USA). The Anisotropic Analytical Algo rithm version 15.6 (Varian Medical Systems, Palo Alto, CA, USA) was used for dose calculation in TPS. Highenergy 6MV photon beams were used in planning and all data of approved plans were digitally transferred to Varian Clinac 2300 CD linear accelerator (M/s Varian Medical Systems, Palo Alto, CA, USA).
Target volume delineation
The Radiation Therapy Oncology Group breast cancer
atlas was used to define the planning target volume.
The heart was defined as all visible myocardium,
the apex, the right auricle, atrium, and infundibulum
of the ventricle. The pulmonary trunk, the root of the
ascending aorta, and superior vena cava were excluded
from the study. The ipsilateral lung volume was
contoured, with the exclusion of the hilum, trachea,
pulmonary vessels, and aortic branches. The spinal
cord was contoured according to the bony limits of
the spinal canal.
Dose prescription
The prescription dose and fractionation were 40Gy in
15 fractions, five fractions/week and 40Gy in 15 fractions
to SCF for PMRT, and 40Gy in 15 fractions followed
by 12.5Gy in five fractions electron beam boost
to lumpectomy tumor cavity. The dose constraints for
the treated volumes were a minimum of 90% and a
maximum of 110% of the prescribed dose.
RT technique
The RT was performed using the two-field standard
tangential technique (n=25) or three-field technique
(n=35). All of the patients treated with the two-field
technique had undergone lumpectomy. PMRT was
done with three-field technique.
Doses calculations and adjustments in beams weight, wedges, blocks, and beam orientations were made as desired in an interactive fashion. Beam orientations were selected and beams were 3D-shaped using multi leaf collimators based on the projection of the structures of interest as seen with beam's-eye view. Setup instructions including field size, gantry, collimator, and table position were provided to facilitate the implementation of treatment beams at the physical simulator and treatment machine.
Plan evaluation
The sparing of OAR (lung, heart, and spinal cord) was
evaluated by comparing their mean doses, lung V10Gy
(volume of lung receiving more than 10Gy), lung V20Gy,
lung V30Gy, heart V25Gy (volume of heart receiving more
than 25Gy), and maximum dose to spinal cord.
Calculation of the NTCP
Using the dose calculation data, we derived the DVH
curves of each OAR. For each patient and structure,
a cumulative DVH was exported from Eclipse with
a bin size of at most 5 cGy and imported into third
party program R studio. Here, NTCP calculations explained
below were performed using DVH metrics
vignette.[13,14]
From these DVH curves, we performed the NTCP calculations for each NTCP model, the Lyman-Kutcher- Burman (LKB) model for radiation-induced pneumonitis, and pericarditis. The equivalent uniform dose (EUD) method was used for reducing the DVH curves to a single dose. The Relative Seriality (RS) model was used for calculation of the NTCP for late cardiac mortality. The LKB NTCP and RS models used in this study are briefly described below.[15-18]
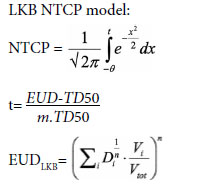
Where TD50 is the 50% tolerance dose at 5 years; EUD is the EUD; n and m are tissue-specific parameters; Di is the dose element, and Vi is the volume element. The parameters for complication of radiationinduced pneumonitis are TD50=24.5, n=0.87.
RS model for late cardiac mortality:
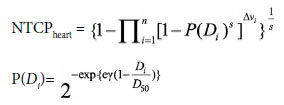
Where D_50=TD50 (=52.3Gy); s is the RS factor (=1), and ? is the maximum relative slope (=1.28).
The CLD is defined as the perpendicular distance from the posterior edge of the tangential field to the posterior part of the anterior chest wall in the middle of the field. Maximum Heart Distance (MHD) is the maximum distance of the heart contour to the posterior field border measured in the beam's eye view of the medial tangential fields.
Before calculation, DVH data were converted to the dose biologically effective to 2 Gy per fraction irradiation, using linear-quadratic model (α/β was equal to 3 Gy for both lung and heart). For the left lung, clinical pneumonitis of grade greater than 2 was used as endpoint in NTCP calculation. In the case of heart, NTCP calculation endpoint was excessive cardiac mortality in the irradiated patients with the left-sided breast cancer. The RS model coefficients used for lung and heart NTCP calculation in this study were obtained from data analysis of patients with breast cancer by Gagliardi et al.[11] In each plan, we calculated the NTCP of RP and cardiac toxicity as described above. We evaluated the change in NTCP values of RP between 3 cm and 4 cm of the CLD. For evaluating the change in NTCP by the MHD, we also measured the MHD in every treatment plan.
Statistical Analysis
Data were compiled using Microsoft Excel and analyzed
using the Statistical Package for the Social Sciences
(SPSS) software version 20.0 (SPSS Inc, Chicago,
IL, USA). The mean and standard deviation of quantitative
variables was calculated. The mean between two
groups was compared using independent t-test. Quantitative
discreet variables were compared using the Chisquare
test. The correlation coefficient was estimated to
assess the relationship between CLD and MHD with
NTCP. P<0.05 was considered statistically significant
and p<0.01 was considered highly significant.
Results
This prospective analytical study included 60 breast cancer patients who have received RT using the twofield standard tangential technique or three-field technique (Table 1).The present study attempted to evaluate dose-volume histogram of heart, lung, and spinal cord in 3DCRT, to analyze adherence of plan with QUANTEC dose constraints. Mean dose for lung was 17.49 Gy, and V20Gy was 39.88%. Mean dose for heart was 12.31 Gy and spinal cord maximum dose was 0.78 Gy. However, the test of significance observed no statistical difference in the mean dose for heart, lung, and spinal cord among patient receiving two-field or three-field radiation therapy (p>0.05) (Table 2).
Table 2 Dose distribution to organs at risk (Lung, Heart, and Spinal Cord)
In the present study, the average lung NTCP for radiation pneumonitis was 3.11%. The risk of radiation pneumonitis was observed to be significantly greater in three-field radiation technique as compared to two fields for lung (p<0.05). Hence, late cardiac mortality probability for heart did not vary significantly between two-field and three-field technique, but average heart NTCP was 2.42%, as shown in Table 3.
The NTCP in the ipsilateral lung revealed a significant difference as the CLD increased from 3 cm to 4 cm (p=0.0012), as shown in Table 4. The NTCP in the heart did not reveal a significant difference as the MHD increased from 2 cm to 3 cm (p=0.05) (Table 5).
The present study observed the statistically significant correlation of MHD and NTCP, that is, as the MHD increased, the NTCP also increased in both twofield and three-field radiation therapy (p<0.00001 and p=0.000402), as depicted in Figure 1. The correlation of CLD was observed to be significant with three-field radiations, that is, as the CLD increased risk of organ damage to lungs increased (p=0.00022), as depicted in Figure 2.
In the present study, correlation of CLD and MHD with dose-volume histogram was observed to be statistically significant (p=0.001). For the breast the slope of the V10Gy, V20Gy and V30Gy were nearly constant, as illustrated in Figure 3.
The analysis for the heart DVH was reflected through the heart volume V25Gy plotted versus MHD. The MHD was observed to be significantly correlated with dose-volume histogram (p<0.001), as depicted in Figure 4.
Fig. 4. Correlation of dosimetric parameters for heart with MHD.
MHD: Maximum heart distance.
Discussion
This study aimed to estimate the doses of irradiation to the OAR in 3D-CRT and also to evaluate if two-dimensional (2D) radiographic parameters such as CLD and MHD have a role in predicting the lung and heart volume at different dose levels.RT has become the essential modality of treatment in post-operative cases of locally advanced breast cancer.[19] The 3D-CRT has been replacing the 2D conventional planning techniques, but 2D techniques are still most common in the developing world. The main advantages of 3D-CRT are both the evaluation of target volume coverage as well as assessing the OAR doses that are essential in predicting the risk of radiation toxicities.[20]
QUANTEC suggested <20% chance of symptomatic pneumonitis with if <30% of lung received 20Gy (V20<=30%), whereas in the present study, V20Gy was 39.88%. The mean dose in the present study was 17.49Gy. QUANTEC suggested 10% and 20% symptomatic pneumonitis at the mean dose of 13 Gy and 20 Gy, respectively.
Similarly, for heart mean dose given in the present study was 12.31 Gy, however, QUANTEC proposed 26 Gy, so it corresponds to QUANTEC constraint. Spinal cord maximum dose is 0.78 Gy which is way lower than QUANTEC constraint of 50 Gy for 0.2% myelopathy rate. However, test of significance observed no statistical difference in mean dose for heart, lung, and spinal cord among patient receiving two-field or three-field radiation therapy (p>0.05).[11]
In the present study, the average lung NTCP for radiation pneumonitis was 3.11%. The risk of radiation pneumonitis was observed to be significantly greater in three-field radiation technique as compared to two fields for lung (p<0.05). The rationale behind this effect is due to the presence of the anterior supraclavicular field, which elevates radiation dose in lung parenchyma that lies beneath the chest wall. The findings of our study are similar to the findings of study conducted by Noh et al.[12] They documented the NTCP of radiation- induced pneumonitis to be 0.5% and it was higher in reverse hockey stick method followed by three fields and least in two fields (0.0%, 0.0%, 3.1%, p<0.001). A study by Das et al.[21] also reported higher risk of RP in three fields as compared to two field. These results are consistent with our NTCP calculations, suggesting that the LKB NTCP model with a reference parameter set may be useful for predicting RP.
In the present study, late cardiac mortality probability for heart did not vary significantly between two-field and three-field technique, but average heart NTCP was 2.42%. These findings were similar to the findings of study conducted by Noh et al.[12], in which they observed NTCP of cardiac mortality as 0.7%. NTCP of cardiac mortality was significantly higher in reverse hockey stick method with no difference in three fields and two fields (0.0%, 0.0%, 3.1%, p<0.001) similar to finding of our study.[17]
Hurkmans et al.[22] reported NTCP values for excess cardiac mortality due to acute myocardial ischemia (MI) with minimum and maximum values of 0.1 and 7.5% (locoregional and tangential RT) and 0.0 and 6.1% (tangential technique). Another study reported an increased incidence of MI in case of the left side RT (p=0.02).[23]
The CLD is commonly used as a simple parameter to assess irradiated lung volume. We observed that as the CLD increased from 3 cm to 4 cm, risk of organ damage ipsilateral lung as revealed by NTCP increased (p<0.01). Furthermore, a statistically significant correlation of CLD and NTCP was established, as the CLD increased, the NTCP also increased (p<0.001) in three-field radiation therapy (p<0.001) but not in two-field technique. This finding is suggestive of the fact that chances of occurrence of pneumonitis in the three-field radiation technique are highly dependent on the CLD; probably, the supraclavicular field in the three-field method increases the irradiated lung volume. Noh et al.[12] also observed increased in NTCP of RP as the CLD increased.
The MHD is a radiographic parameter that helps to measure the irradiated heart volume for each patient. Hurkmans et al.,[22] in their study, used RS model for predicting NTCP of cardiac mortality and suggested a cardiac mortality curve equation based on MHD. Our study observed that as the MHD increased from 2 cm to 3 cm, the NTCP heart also increased (p<0.01). Furthermore, we observed that a statistically significant correlation of MHD and NTCP was established, which means that as the MHD increased, the NTCP also increased (p<0.001) both two-field and three-field radiation therapy (p<0.001). Similar to the findings of present study, Noh et al.[12] also observed increased in NTCP of radiation- induced cardiac mortality as the MHD increased.
In the present study, correlation of CLD with DVH was observed to be statistically significant. For the breast, the slope of the V10Gy, V20Gy, and V30Gy was nearly constant. Das et al.[21] observed findings similar to our study and concluded that the correlation of treatment parameters (CLD) provides a direct link to the volume of the lung treated to a given dose. Another retrospective study by Teh et al.,[24] to correlate DVH with RP observed the occurrence of steroid requiring RP after 6 months and the overall incidence of RP was 1.1%. In contrast to our study, Minor et al.,[25] in their retrospective study of 353 patients, observed no correlation between CLD and pneumonitis.
In the present study, correlation of MHD with DVH was observed to be statistically significant. The analysis for the heart DVH was reflected through the heart volume V25Gy plotted versus MHD. The MHD was observed to be significantly correlated with DVH. Das et al.[21] study findings were similar to our study and suggested positive correlation of treatment parameters (MHD) with volume of heart treated to a given dose. Contrasting findings were observed by Borger et al.,[26] in which they assessed the risk of cardiovascular disease (CVD) after adjuvant radiation. They did not find any significant correlation between MHD and NTCP heart.
An accurate absolute NTCP model of excessive late cardiac mortality and RP requires accurate clinical data. However, several factors limit the accuracy of these models. These include a long latency period before clinical complications arise, the relatively low incidence of radiation-induced cardiac complications with newer RT techniques, and the relatively high prevalence of ischemic heart disease in the general population and the absence of good dosimetric and volumetric data in retrospective studies. Although the absolute NTCP values should be viewed with caution, they must be fitted to clinical outcome data and then are useful approximations of risk. This study is limited in that it does not consider many other risk factors of cardiovascular diseases, such as a history of hypertension, smoking, and use of combined cardiotoxic chemotherapy.
Conclusion
We did not analyze the actual clinical data of complications in this study; hence, it is difficult to apply our results directly to the clinic. However, our results are useful to reanalyze the previous 2D-based clinical reports about breast RT complications as a viewpoint of the NTCP.Peer-review: Externally peer-reviewed.
Conflict of Interest: All authors declared no conflict of interest.
Ethics Committee Approval: The study was approved by the Gandhi Medical College, Bhopal Ethics Committee (no: 3827-29/MC/IEC/2018, date: 30/01/2018).
Financial Support: None declared.
Authorship contributions: Concept - O.P.S., V.Y.; Design - O.P.S., V.Y., R.S.; Supervision - S.Y., P.K.P.; Funding - V.Y., S.Y.; Materials - R.S., H.U.G., V.T.; Data collection and/or processing - R.S., M.C., S.S.; Data analysis and/or interpretation - R.S., V.Y., P.K.P.; Literature search - O.P.S., V.Y., R.S.; Writing - R.S., V.Y.; Critical review - O.P.S., V.Y.
References
1) Mathur P, Sathishkumar K, Chaturvedi M, Das P,
Sudarshan KL, Santhappan S, et al; ICMR-NCDIRNCRP
Investigator Group. Cancer Statistics, 2020:
Report From National Cancer Registry Programme,
India. JCO Glob Oncol 2020;6:1063-75
2) Whelan TJ, Julian J, Wright J, Jadad AR, Levine ML.
Does locoregional radiation therapy improve survival
in breast cancer? A meta-analysis. J Clin Oncol
2000;18(6):1220-9.
3) Early Breast Cancer Trialists" Collaborative Group.
Favourable and unfavourable effects on long-term survival
of radiotherapy for early breast cancer: an overview
of the randomised trials. Lancet 2000,355(9217):1757-70.
4) Darby SC, Ewertz M, McGale P, Bennet AM, Blom-
Goldman U, Brønnum D, et al. Risk of ischemic heart
disease in women after radiotherapy for breast cancer.
N Engl J Med 2013;368(11):987-98.
5) Harris EE, Correa C, Hwang WT, Liao J, Litt HI, Ferrari
V, et al. Late cardiac mortality and morbidity in
early-stage breast cancer patients after breast-conservation
treatment. J Clin Oncol 2006;24(25):4100-06.
6) Taylor CW, Nisbet A, McGale P, Darby SC. Cardiac
exposures in breast cancer radiotherapy: 1950s-1990s.
Int J Radiat Oncol Biol Phys 2007;69(5):1484-95.
7) Chargari C, Kirov KM, Bollet MA, Magne N, Vedrine
L, Cremades s, et al. Cardiac toxicity in breast cancer
patients: From a fractional point of view to a global
assessment. Cancer Treat Rev 2011;37(4):321-30.
8) Magné N, Chargari C, MacDermed D, Conforti R,
Vedrine L, Spano JP, et al. Tomorrow"s targeted therapies
in breast cancer patients: What is the risk for
increased radiation-induced cardiac toxicity? Critical
Rev Oncol Hematol 2010;76(3):186-95.
9) Roychoudhuri R, Robinson D, Putcha V, Cuzick J, Darby
S, Møller H. Increased cardiovascular mortality more
than fifteen years after radiotherapy for breast cancer: a
population-based study. BMC Cancer 2007;7:9.
10) Demirci S, Nam J, Hubbs JL, Nguyen T, Marks LB.
Radiation-induced cardiac toxicity after therapy for
breast cancer: interaction between treatment era
and follow-up duration. Int J Radiat Oncol Biol Phys
2009;73(4):980-87.
11) Gagliardi G, Constine LS, Moiseenko V, Correa C,
Pierce LJ, Allen AM, et al. Radiation dose?volume effects
in the heart. QUANTEC: Organ Specific Paper.
Int J Radiat Oncol Biol Phys 2010;76(3):S77-S85.
12) Noh OK, Park SH, Ahn SD, Choi EK, Lee SW, Song SY, et
al. Probabilities of pulmonary and cardiac complications
and radiographic parameters in breast cancer radiotherapy.
J Korean Societ Radiol Oncol 2010;28(1):23-31.
13) R Development Core Team. R: A language and environment
for statistical computing. Vienna, Austria: R
Foundation for Statistical Computing; 2015.
14) Wollschläger D, Karle H. DVHmetrics: Analyze dosevolume
histograms and check constraints, 2015. Available
at: http://CRAN.R-project.org/package=DVHmetrics.
Accessed Nov 11, 2022.
15) Marks LB, Yorke ED, Jackson A, Ten Haken R, Contine
LS, Eisbruch A, et al. Use of normal tissue complication
probability models in the clinic. Int J Radiat
Oncol Biol Phys 2010;76(3):10-9.
16) Kutcher GJ, Burman C, Brewster L, Goitein M, Mohan
R. Histogram reduction method for calculating complication
probabilities for three-dimensional treatment
planning evaluations. Int J Radiat Oncol Biol
Phys 1991;21(1):137-46.
17) Lyman JT. Complication probability as assessed from
dose-volume histograms. Radiat Res 1985;104(2s):13-9.
18) Gagliardi G, Lax I, Ottolenghi A, Rutqvist LE. Longterm
cardiac mortality after radiotherapy of breast
cancer- application of the relative seriality model. Br J
Radiol 1996;69(825):839-46.
19) Recht A. Integration of systemic therapy and radiation
therapy for patients with early-stage breast cancer
treated with conservative surgery. Clin Breast Cancer
2003;4(2):104-13.
20) Onal C, Oymak E, Kotek A, Efe E, Arslan G. Correlation
of conventional and conformal plan parameters
for predicting radiation pneumonitis in patients treated
with breast cancer. J Breast Cancer 2012;15(3):320?28.
21) Das IJ, Cheng EC, Schultz DJ, Harris EE, Solin LJ.
Radiation pneumonitis in megavoltage beam treatment
of breast cancer. Int J Radiat Oncol Biol Phys
2001;51(3):245-6.
22) Hurkmans CW, Cho BC, Damen E, Zijp L, Mijnheer
BJ. Reduction of cardiac and lung complication probabilities
after breast irradiation using conformal RT
with or without intensity modulation. Radiother Oncol
2002;62(2):163-71.
23) Paszat LF, Mackillop WJ, Groome PA, Schulze K,
Holowaty E. Mortality from myocardial infarction following
postlumpectomy radiotherapy for breast cancer:
A population-based study in Ontario, Canada. Int
J Radiat Oncol Biol Phys 1999;43(4):755-62.
24) Teh AY, Park EJ, Shen L, Chung HT. Three-dimensional
volumetric analysis of irradiated lung with adjuvant
breast irradiation. Int J Radiat Oncol Biol Phys
2009;75(5):1309-15.





