Summary
OBJECTIVETo compare the dosimetric criteria of intensity-modulated radiotherapy (IMRT) and volumetric modulated radiotherapy (VMAT) plans with simultaneous integrated boost (SIB) technique in cervical cancer patients with para-aortic lymph node (PALN) metastases.
METHODS
SIB-IMRT and SIB-VMAT plans of 10 patients were retrospectively analyzed. The elective volume
received 45 Gy(PTV45) in 25 fractions of 1.8 Gy, while the integrated boost volume (lymph nodes)
simultaneously received 55 Gy (PTV55). Using the same dose constraints in optimization, IMRT
plans consisted of 9 fields, while VMAT plans were performed with 2 full arcs. Volume and dose
parameters were determined across the planning target volume, bladder, bowel, femoral heads,
kidneys, liver, rectum, sigmoid, and spinal cord. Conformity and homogeneity indices were calculated,
the Monitor Unit (MU) was analyzed, and the Wilcoxon-signed rank test was applied for
statistical analysis (p?0.05).
RESULTS
Both techniques were found to be effective for treatment, but there was a significant difference in favor
of SIB-VMAT in terms of target volume reaching the predicted dose and protection of critical organs
(OAR) (p=0.028). For PTV55, MU and right-left kidney; V20, V30 - V20, V30, liver; Dort, liver values were
significantly different (p=0.005, p=0.005, p=0.005, p=0.02, p=0.005, p=0.007, p=0.03, respectively). In
SIB-IMRT, a significant difference was observed for CI value close to 1 (p=0.02).
CONCLUSION
The SIB-VMAT technique showed lower MU, kidney, and liver values, and SIB-IMRT showed better
CI values. Other parameters indicated that the two planning techniques were nearly equivalent. These
findings indicate the different efficacies of treatment techniques in radiotherapy planning for cervical
cancer patients who were diagnosed with PALN metastases.
Introduction
Cervical cancer is a prevalent malignancy in women, ranking fourth worldwide based on the 2020 Global Cancer Observatory statistics (GLOBOCAN). This disease ranks 12th in our country, with an incidence rate of 4.8 per thousand, as reported in the literature.[1,2] Radiotherapy represents a pivotal treatment modality, especially in cases with lymph node metastasis. As chemotherapy technology evolves, radiotherapy has emerged as the standard treatment approach. In cases where metastasis has occurred in the paraaortic lymph nodes, careful evaluation of all volumes and organs at risk is critical to ensure treatment success with minimal side effects while providing a uniform dose distribution within the target volume.[1-3] Thankfully, advancements in radiotherapy techniques have improved treatment outcomes. While three-dimensional conformal radiotherapy (3DCRT) was commonly used in the past, the latest techniques such as intensity-modulated radiotherapy (IMRT) and volumetric-modulated radiotherapy (VMAT) have grown in popularity due to their ability to offer fewer fractions, shorter treatment times, and high fraction doses.[4-6] These techniques have also shown promise in studies involving gynecologic cancers, as they cause less damage to normal tissues, reduce treatment times, and require fewer monitor units.[7,8]Recent research has focused on comparing IMRT and VMAT techniques for simultaneous integrated boosts (SIB) in various anatomical sites. This is because the clinical use of VMAT has increased.[9,10] However, there is still a lack of comprehensive studies evaluating these techniques, particularly in cases of cervical cancers with paraaortic lymph node (PALN) metastases.[11,12]
The focus of our research was on conducting a comparative analysis of the dosimetric aspects of IMRT and VMAT plans under SIB conditions to determine the optimal treatment approach for patients undergoing radiotherapy. We sought to evaluate the effectiveness of SIB-VMAT and SIB-yttrium-90 radioembolization (SIB-YART) treatment planning methods for cervical cancer patients, focusing on the Planned Target Volume (PTV) and doses received by organs at risk. To achieve this, we conducted a statistical analysis of the dose volume histograms (DVH) generated by both techniques, comparing their respective dosimetric properties.
Methods
This research involved 10 patients who had been diagnosed with cervical cancer with PALN metastasis and had completed their treatment, with the Department"s consent. Written consents required for the study were obtained in compliance with the Declaration of Helsinki, and approval was granted by the local ethics committee (Decision No: 24-2.1T/75).In order to ensure comprehensive treatment, all patients underwent a pelvic-paraaortic field plan. A radiation oncologist utilized computed tomography (CT) scans of the pelvic region from ten patients to create the PTV. The plan incorporated definitions of the gross tumor volume (GTV), clinical target volume (CTV), internal tumor volume (ITV), and contours relating to critical organs (OAR), for instance, bladder, bowel, femoral heads, kidneys, liver, rectum, sigmoid, and spinal cord. The PTV was designed with a margin of 1.0 cm for the CTV and 1?1.5 cm for the ITV, allowing organ movement while limiting the dose to normal tissues.
The planned dose for the elective volume was 45 Gy delivered in 25 fractions of 1.8 Gy each, and the integrated boost volume was planned to administer 55 Gy over the same 25 fractions of 2.2 Gy simultaneously. The Eclipse Treatment Planning System was utilized to create SIB-IMRT and SIB-VMAT plans with 6-MV photon beams from a Varian TrueBeam STX linear accelerator in California, USA. The IMRT plans were optimized using the dose volume optimizer, while the VMAT plans utilized the progressive resolution optimizer. Both plans were calculated using the AcurosXB planning algorithm (version 1610). In the creation of IMRT plans, the sliding window algorithm application method was employed, utilizing nine planar equal fields placed at varying degrees around the patient. For the VMAT plan, two coplanar arcs of 360 degrees were utilized with the same isocenter. Both plans were normalized to obtain a minimum of 95% of the prescribed dose and thoroughly evaluated based on the resulting parameters. Both plans utilized identical planning targets for every patient. The numerical target table was populated with the same objectives for optimizing IMRT and VMAT plans. The primary focus during dose delivery was to guarantee that 95% of the prescribed dose reached the PTV, followed by minimizing the dosage to critical organs like the kidneys, and finally, administering lower doses to other OAR structures to reduce the dosage to critical organs to the fullest extent possible. The plans for both techniques were developed to yield optimal outcomes for 10 patients. DVH was used to analyze dose values to evaluate the quality of each plan for PTV (elective and SIB). These values included the minimum, maximum, and mean doses for OAR, and additionally assessed the volume that receives 95% of the prescribed dose and the maximum doses received by 2%, 50%, and 98% of the volume. From these values, the literature determined the homogeneity index (HI) and conformity index (CI) for individual plans. A small HI value indicates a consistent dose distribution across the volume, while a CI value nearing 1 indicates a high degree of conformity in the delivery of the dose to healthy tissues surrounding the target volume. The formulas for these expressions are:
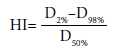
Regarding radiation dosage, D2% is the dosage in the target volume, also known as the 2% target volume dose. D98% refers to the minimum dosage within the target volume, or the 98% target volume dose. Meanwhile, D50% pertains to the average radiation dose received in a tumor, which encompasses up to fifty percent of the volume designated as the target. If the HI value is low, this indicates that the dose distribution within the volume is homogeneous.
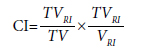
The TVRI refers to the volume intended to receive radiation treatment and is surrounded by a reference isodose. Meanwhile, TV pertains to the target volume, while the VRI parameter defines the volume of the reference isodose. A CI value nearing 1 indicates a reduced radiation dose to the tissues surrounding the target volume, as supported by previous studies.[7,13,14]
In order to compare the OAR sparing ability of SIB-IMRT and SIB-VMAT plans, we analyzed the volumes of the bladder, bowel, femoral heads, liver, rectum, sigmoid, and kidneys using using V70(%), V195(cc), V15(%), V30(%), V40(%), V40(%), V55(%),V32(%) V30(%), V20(%). Additionally, we examined mean dose values of 18 Gy and 32 Gy for kidneys and liver, and the maximum dose limit of 45 Gy for the spinal cord. Previous research has indicated that VMAT may produce lower MU values compared to IMRT due to less radiation leakage through collimator leaves and reduced neutron production at high energies. As such, we recorded technique-specific MU values for our study aims to assess the efficacy of each technique.[7,14,15] We utilized the Wilcoxon paired two-sign rank test to perform a statistical evaluation on nonparametrically distributed data. A significant difference was indicated if the p-value equaled or fell below 0.05 (p≤0.05).[16]
Results
All 9 patients achieved the SIB targets for PTV coverage and OAR sparing with the SIB-IMRT and SIB-VMAT plans. However, the IMRT plan for one patient failed to achieve its target due to inadequate use of the 9 fields in treatment. On the other hand, the VMAT plan successfully achieved the SIB targets. Each plan was designed to be clinically feasible. The techniques showed statistically significant differences in MU, kidney, and liver values.The comparison results of Tables 1 and 2 depict SIB planning utilizing IMRT and VMAT techniques. Table 1 focuses on the parameters of SIB-IMRT and SIB-VMAT for PTV55 coverage, while Table 2 presents the performance of the two techniques regarding OAR preservation. In Table 1, SIB-VMAT outperforms SIBIMRT in terms of MU (545.91), CI (0.74), and HI (0.04), although the HI results are not statistically significant. Conversely, Table 2 indicates that SIB-VMAT is significantly superior to SIB-IMRT in preserving OAR in the right kidney V30(%), V20(%), left kidney V30(%), V20(%), and liver Dort(Gy) values with 9.83%, 9.26%, 8.15%, 7.64%, and 7.74Gy values, respectively
In Figure 1, a and b are the isodose distributions of both the SIB-IMRT and SIB-VMAT plans for a patient in the transversal section (top), along with the isodose distributions of the same patient's treatment plans in the frontal section (bottom). Additionally, Figure 2 showcases the PTV and OAR DVRs of the pertinent parameters in the patient"s SIB-IMRT and SIB-VMAT plans, highlighting the defined criteria in varying colors.
Discussion
Cervical cancers are highly treatable, and thanks to advances in technology and medicine, survival rates are on the rise. Radiotherapy is a critical element in treating cervical cancer, and treatment plans are established according to the stage of the disease and the extent of lymphatic spread.[17] This study aimed to compare treatment plans using the SIB technique with those using IMRT and VMAT techniques in 10 patients with cervical cancer and PALN metastasis. Precise planning and dosimetric measurements are crucial in radiotherapy treatments, and techniques like IMRT and VMAT take into account the structure of the target area to minimize side effects while regulating radiation doses. Studies have shown that SIB-assisted VMAT and IMRT treatment plans produce more favorable outcomes.[18,19]The preferred parameters to evaluate the two techniques are HI, CI, and MU.[1,5,20] Wu et al.[1] conducted a comparison of 2-arc VMAT and 9-field IMRT techniques for 20 patients, using dose values of 45 and 50.4 Gy. They observed a notable disparity between the techniques in HI value (p=0.036). On the other hand, Vergalasova et al.[20] did not identify a statistically significant disparity in HI criteria in their study comparing two techniques for 20 patients (p=0.55). In our research, we observed that the SIB-IMRT technique showed superiority with an HI value of 0.04, although no significant discrepancy was found for HI (p=0.08). In Wu et al.[1]'s study comparing the same techniques, they obtained a CI value close to our IMRT result (0.77) with the prescription dose values they chose (45 Gy and 50.4 Gy) and established a significant difference among the techniques (p=0.016). In a study carried out by Cheng et al.[5] with 10 patients, the CI criterion revealed a significant difference (p=0.001). Upon analyzing the CI values, researchers found that the SIB-IMRT technique was inferior with an assessment of 0.74, and there was a significant variance compared to the results of the SIB-VMAT technique (p=0.02). Wu et al.[1] discovered that the VMAT technique exhibited superiority in the MU value, and there was a statistically significant difference observed when compared to other techniques (p=0.001). Meanwhile, Vergalasova et al.[20]'s study noted a statistically significant difference for the MU criteria (p=0.00009) when comparing the two techniques. In our research, we observed a significant difference when analyzing the MU values between the SIB-VMAT and SIB-IMRT techniques, with the former proving statistically superior (p=0.005).
In a comparative study conducted by Riou et al.[14] it was found that the SIB-VMAT technique was superior for bladder dose limit values in 10 patients. Conversely, no statistically significant difference was found between the SIB-VMAT and SIB-IMRT techniques. Similar findings were reported by Vergalasova et al.[20] who found no statistically significant difference in bladder criteria in their study (p=0.19). When we look at the bladder values obtained in our assessment, we identified no significant difference between SIB-VMAT and SIB-IMRT (p=0.13). In the QUANTEC protocols examined, the bowel limit was determined to be <195 cc.[21] The exact limits were applied in this study, and no significant difference was observed in the comparison of bowel doses (p=0.13). The RTOG protocols reviewed, and the dose limits for the right-left femoral head were determined as <15% and <15%, respectively.[22] In this study, the dose limits were determined in the same way, and in the comparison made for SIB-IMRT and SIB-VMAT, the values for the right femoral head were 10.79 and 10.94, respectively, with no significant difference for p=0.16, and the values for the left femoral head were 9.76 and 11.62, respectively, with no statistically significant difference (p=0.24). Wu et al.[1] found that the VMAT technique showed superiority for the mean left-right kidney values with a significant difference between the techniques (p=0.001, p=0.001, respectively). However, Vergalasova et al.[20] identified no significant discrepancy in mean left-right kidney values. In the comparison of mean left-right kidney doses between SIB-VMAT and SIB-IMRT, no notable difference was found for the left kidney, while a significant difference was found for the right kidney doses (p=0.17, p=0.39, respectively). In the examination of mean left-right kidney doses between SIB-VMAT and SIB-IMRT, no significant difference was established for the left kidney, while a significant difference was found for the right kidney doses (p=0.07, p=0.05, respectively). In the examined QUANTEC protocols, the liver limit value was determined as <32 Gy.[21] In this study, the same limits were used, and there was no statistically significant difference between the two techniques for liver mean doses (p=0.09). Wu et al.[1] found that the VMAT technique was superior for rectum value, and there was a significant difference between the techniques (p=0.001). Cheng et al.[5] found a significant difference between the rectum values of the two techniques in their study (p=0.001). In our research, although there was no significant difference between the two techniques for rectal values, percent doses showed superiority in favor of the SIB-VMAT technique (p=0.95). In their comparison study of 8 patients, Jin et al.[9] found the SIB-VMAT technique superior for spinal cord dose limit values, and a significant difference was found between the two techniques (p=0.04). However, in our study, dose limits were determined similarly, though no statistically significant difference was detected in the comparison made for the spinal cord (p=0.09). Based on the OAR dose data collected in the study, the SIB-VMAT technique demonstrated superiority in the average values of the right kidney, left kidney, and liver, while remaining within the specified limits. A significant difference was observed between the two techniques. The SIB-IMRT technique showed superiority in the average value of the left kidney, and a significant difference was also detected.
When choosing between the SIB-IMRT and SIBVMAT techniques, it is important to consider various factors, such as the patient's condition and treatment duration. Although VMAT has advantages in terms of treatment duration, it requires more time for treatment planning and quality assurance. However, some studies suggest that quality assurance plans are quicker with VMAT.[9,23]
Conclusion
Our study revealed that both VMAT and IMRT techniques exhibit distinct advantages and disadvantages. Therefore, the selection of the most suitable technique should be based on the patient"s condition and treatment planning. Our current research unveiled that although there was a significant difference in SIB-IMRT and SIBVMAT plans among 10 patients, both techniques provided similar dosimetric results. Accordingly, it is crucial to consider factors, particularly the patient's condition, clinical equipment, and the expertise of doctors and physicists, when selecting the appropriate technique. Our results indicate that both SIB-IMRT and SIB-VMAT techniques are effective in treating cervical cancer. Ethics Committee Approval: The study was approved by the Ege University Medical Research Ethics Committee (no: 24-2.1T/75, date: 22/02/2024).Authorship contributions: Concept - İ.A.E., H.E., Z.Ö.; Design - İ.A.E., H.E.; Supervision - İ.A.E., H.E., N.O., Z.Ö.; Funding - İ.A.E., H.E.; Materials - İ.A.E., H.E.; Data collection and/or processing - İ.A.E., H.E.; Data analysis and/or interpretation - İ.A.E., H.E., N.O.; Literature search - İ.A.E., H.E., N.O.; Writing - İ.A.E., H.E., Z.Ö.; Critical review - İ.A.E., H.E., N.O., Z.Ö.
Conflict of Interest: All authors declared no conflict of interest.
Use of AI for Writing Assistance: Not declared.
Financial Support: None declared.
Peer-review: Externally peer-reviewed.
References
1) Wu Y, Zhu B, Han J, Xu H, Gong Z, Yang Y, et al. A comparative
dosimetric study of cervical cancer patients with
para-aortic lymph node metastasis treated with volumetric
modulated arc therapy vs. 9-field intensity-modulated
radiation therapy. Ann Transl Med 2019;7(22):675.
2) Bhatla N, Aoki D, Sharma DN, Sankaranarayanan R.
Cancer of the cervix uteri: 2021 update. Int J Gynaecol
Obstet 2021;155(Suppl 1):28-44.
3) Aydoğdu SGM, Özsoy Ü. Serviks kanseri ve HPV. Androl
Bul [Article in Turkish] 2018;20:25-9.
4) Swamidas J, Pradhan S, Chopra S, Panda S, Gupta Y,
Sood S, et al. Development and clinical validation of
Knowledge-based planning for Volumetric Modulated
Arc Therapy of cervical cancer including pelvic and para
aortic fields. Phys Imaging Radiat Oncol 2021;18:61-7.
5) Cheng JY, Huang EY, Hsu SN, Wang CJ. Simultaneous
integrated boost (SIB) of the parametrium and
cervix in radiotherapy for uterine cervical carcinoma:
A dosimetric study using a new alternative approach.
Br J Radiol 2016;89(1068):20160526.
6) Park JM, Park SY, Kim JI, Kang HC, Choi CH. A comparison
of treatment plan quality between Tri-Co-60
intensity modulated radiation therapy and volumetric
modulated arc therapy for cervical cancer. Phys Med
2017;40:11-6.
7) Cilla S, Macchia G, Sabatino D, Digesù C, Deodato
F, Piermattei A, et al. Applicator-guided volumetricmodulated
arc therapy for low-risk endometrial cancer.
Med Dosim 2013;38(1):5-11.
8) Pedicini P, Caivano R, Fiorentino A, Strigari L, Califano
G, Barbieri V, et al. Comparative dosimetric
and radiobiological assessment among a nonstandard
RapidArc, standard RapidArc, classical intensitymodulated
radiotherapy, and 3D brachytherapy for the
treatment of the vaginal vault in patients affected by
gynecologic cancer. Med Dosim 2012;37(4):347-52.
9) Jin X, Yi J, Zhou Y, Yan H, Han C, Xie C. Comparison
of whole-field simultaneous integrated boost VMAT
and IMRT in the treatment of nasopharyngeal cancer.
Med Dosim 2013;38(4):418-23.
10) Wu S, Lai Y, He Z, Zhou Y, Chen S, Dai M, et al. Dosimetric
comparison of the simultaneous integrated
boost in whole-breast irradiation after breast-conserving
surgery: IMRT, IMRT plus an electron boost and
VMAT. PLoS One 2015;10(3):e0120811.
11) Guerrero M, Li XA, Ma L, Linder J, Deyoung C, Erickson
B. Simultaneous integrated intensity-modulated
radiotherapy boost for locally advanced gynecological
cancer: Radiobiological and dosimetric considerations.
Int J Radiat Oncol Biol Phys 2005;62(3):933-9.
12) Macchia G, Cilla S, Deodato F, Legge F, Di Stefano A,
Chiantera V, et al. Intensity-modulated extended-field
chemoradiation plus simultaneous integrated boost
in the pre-operative treatment of locally advanced
cervical cancer: A dose-escalation study. Br J Radiol
2015;88(1055):20150385.
13) Paddick I. A simple scoring ratio to index the conformity
of radiosurgical treatment plans. Technical
note. J Neurosurg 2000;93 Suppl 3:219-22.
14) Riou O, Regnault de la Mothe P, Azria D, Aillères N,
Dubois JB, Fenoglietto P. Simultaneous integrated
boost plan comparison of volumetric-modulated
arc therapy and sliding window intensity-modulated
radiotherapy for whole pelvis irradiation of locally
advanced prostate cancer. J Appl Clin Med Phys
2013;14(4):4094.
15) Zhao J, Hu W, Cai G, Wang J, Xie J, Peng J, et al. Dosimetric
comparisons of VMAT, IMRT and 3DCRT for
locally advanced rectal cancer with simultaneous integrated
boost. Oncotarget 2016;7(5):6345-51.
16) Ural A, Kılıç İ. Bilimsel araştırma süreci ve SPSS ile
veri analizi. 3th ed. Ankara: Detay Yayıncılık; 2010.
17) Mahmoud O, Kilic S, Khan AJ, Beriwal S, Small W
Jr. External beam techniques to boost cervical cancer
when brachytherapy is not an option-theories and applications.
Ann Transl Med 2017;5(10):207.
18) Boyle J, Craciunescu O, Steffey B, Cai J, Chino J. Methods,
safety, and early clinical outcomes of dose escalation
using simultaneous integrated and sequential
boosts in patients with locally advanced gynecologic
malignancies. Gynecol Oncol 2014;135(2):239-43.
19) Ramlov A, Assenholt MS, Jensen MF, Grønborg C,
Nout R, Alber M, et al. Clinical implementation of
coverage probability planning for nodal boosting in
locally advanced cervical cancer. Radiother Oncol
2017;123(1):158-63.
20) Vergalasova I, Light K, Chino J, Craciunescu O. Simultaneous
integrated boost (SIB) for treatment of gynecologic
carcinoma: Intensity-modulated radiation
therapy (IMRT) vs volumetric-modulated arc therapy
(VMAT) radiotherapy. Med Dosim 2017;42(3):230-7.
21) Bentzen SM, Constine LS, Deasy JO, Eisbruch A,
Jackson A, Marks LB, et al. Quantitative Analyses of
Normal Tissue Effects in the Clinic (QUANTEC): An
introduction to the scientific issues. Int J Radiat Oncol
Biol Phys 2010;76(3 Suppl):S3-9.





