Summary
OBJECTIVEIn this study, we aimed to make dosimetric measurements of the vaginal speculum by producing the upper and lower tongue of the vaginal speculum from polyetheretherketone (PEEK) material and to test its usability in brachytherapy application.
METHODS
A modular structure of the metallic vaginal speculum, which we use in our routine practice, can be easily
separated from the handle of the speculum, has been designed and produced with a 3D printer from
PEEK material with a layer thickness of 200 µ. Dosimetric measurements of speculum tongue made of
PEEK material were made using two different dosimetric methods (three different techniques as the
treatment planning system ACUROS BV and TG43 algorithms, and the Radiochromic Film Dosimetry
system [Gafchromic: EBT3]).
RESULTS
The values obtained by all three methods were correlated with each other and the speculum did not affect
negatively dose distribution in the dose-distance curves. The dose values obtained by using ACUROS
BV and TG43 algorithms at the Dwell position and the dose values obtained in the Gafchromic dosimetry
measurements made at these points were found to be correlated with each other (ACUROS BV vs.
TG43 p<0.001, ACUROS BV vs. EBT3 p=0.008, TG43 vs. EBT3 p=0.006).
CONCLUSION
When all the measurement results were examined, it was seen that the values obtained were correlated
with each other, and no negative effect of the speculum on the dose distribution was observed in the
dose distance curves.
Introduction
Cervical cancer is the fourth most frequent cancer in women globally, second most frequent cancer in women aged 15-44, and it is the fourth most frequent cancer among the reasons for cancer-related deaths.[1,2] Brachytherapy performed after chemotherapy synchronous with external pelvic radiotherapy (RT) is the standard treatment approach in patients diagnosed with locally advanced cervical cancer.[3,4] External pelvic RT is used to treat pelvic lymph nodes, parametrium, and primary tumors while brachytherapy essentially targets the treatment of primary tumors. The addition of brachytherapy treatment to external RT improves both local control and overall survival, and brachytherapy treatment is an indispensable element in the treatment of patients with locally advanced cervical cancer.[5-9]The purpose of brachytherapy treatment is to place radioactive sources near or inside the tumor. This ensures not only increased dosage in the targeted tissues with tumors and improvement of overall survival through local control but also reduced dosages for the bladder, rectum, sigmoid, and other organs at risk (OARs) beyond or near the target.[3] To this end, while radiophysical properties (such as the inverse square rule) of radioactive sources or brachytherapy are exploited, certain manipulations are employed to keep OARs away from the radioactive source or various applicators may be used for the same purpose.[10]
Brachytherapy procedure generally lasts 1.5-2 h and might be implemented under general or spinal anesthesia as the process of placing the applicators inside the cervix, endometrium or tumor may be accompanied by pain or anxiety. During this process, the patient is supposed to lie down and hold still. In brachytherapy applications, it is crucial to select the correct applicator, place it correctly, and then, keep OARs away from the radioactive source. For this purpose, a stainlesssteel vaginal speculum that is available in the market and routinely used is fitted before the applicators are placed into the cervix and uterus. Then, the packing of the vagina is performed using the gauze dipped into normal saline to keep away the bladder in the front and the rectum at the back. After this process is completed, the vaginal speculum which has a modular structure is split into two parts the upper and lower parts, and pulled outside of the vagina.[10] However, the spoonshaped structure of the lower and upper blades poses the greatest problem for the implementer. This spoonshaped structure may cause the gauze placed inside the vagina to be removed as the speculum is pulled outside, damaging the packing.
Polyetheretherketone (PEEK) is one of the outstanding polymers in the semi-crystalline thermoplastic polymer class. Today, PEEK is available in various forms such as fiber, film, resin, fabric, cable, membrane, and composite. Chemically, the PEEK polymer consists of repeating units of one ketone group and two either groups, and it is durable and biologically compatible thanks to its fully aromatic, highly stable, and linear structure that contains only carbon, hydrogen, and oxygen atoms.[11]
The starting point of this study is the possibility of replacing the metal speculum with PEEK so that it can be left in place during gynecologic brachytherapy procedures. Hence, this project aims to modify the vaginal speculum that is currently available in the market and routinely used in daily practice by producing the lower and upper blades of the vaginal speculum using a PEEK material and performing dosimetric measurements, and testing the feasibility of the resulting modification for brachytherapy applications.
Methods
Design of the Blades of the Vaginal Speculum and their Production from a PEEK MaterialAt the beginning of the study, the dimensions and shape of the metallic speculum used in our routine practice were digitized using a 3D drawing software program. Using the digitized images, a modular structure was designed that would allow the lower and upper blades of the vaginal speculum to be easily removed from the body. The upper and lower blades of the designed speculum were produced from the PEEK material with a layer thickness of 200 microns using an Intamsys Funmat HT 3D printer (Intamsys Technology Co. Ltd., Shanghai, China) (Fig. 1).
Fig. 1. Vaginal speculum tongues made of PEEK material.
PEEK: Polyetheretherketone.
Design and Production of the Test Apparatus For dosimetric measurements regarding the radiation permeability of the produced speculum blades, a phantom apparatus was designed and produced with a width of 8×10 cm and a height of 12 cm using the glass material. A guide and locking mechanism were produced from polylactic acid using an Intamsys Funmat HT 3D printer to ensure that the speculum blades and radioactive source can be secured inside the apparatus (Fig. 2a, b).
Performing Dosimetric Measurements
Two different dosimetry methods (treatment planning
system (TPS) and Radiochromic Film Dosimetry
System (GAFChromic: EBT3)) were used to perform
dosimetric measurements of the blades of the vaginal
speculum produced from the PEEK material, and the
values calculated using these two methods were compared
to each other.
Measurements Made using the TPS
The Eclipse TPS (Version: 15.6, Varian Medical Systems,
Palo Alto, United States of America) was used
as the TPS. In dosimetric comparisons, computed
tomography (CT) (Siemens Somatom AS, Siemens
Healthineers, Erlangen, Germany) of the test apparatus was taken first. The guiding tube (bar) with code
no. GM11011180 of the cylinder applicator with code
no. GM11011100 of the Varian GammaMed Plus iX
brachytherapy device (Varian Medical Systems, Palo
Alto, United States of America) was placed at the center
of the testing apparatus. To enable measurements with
and without the speculum in the test apparatus, one
blade of the speculum was placed 2.3 cm away from
the applicator to the left of the source and no speculum
blade was placed to the other side. This point was chosen
because it is the distance at which a dose of 3 Gy is
delivered in the TPS. Here, the aim was to perform dosimetric
measurements from different directions and
compare them. After these processes, water was placed
inside the test apparatus as representative of soft tissue.
For dose calculations, the Acuros BV calculation
algorithm (Varian Medical Systems, Palo Alto, United
States of America), which takes Hounsfield units in
TG43 and CT images, into consideration, was used.
Dose values at the specified points at the sides with and
without the speculum (the points where GAFChromic
films will be placed) on the images sets obtained from
CT were recorded using the beam data and calculation
algorithm belonging to 192lr (t1/2: 73.827 days) previously
loaded into the system. On both sides, the points
were set 5.02 (LEFT), 4.07 (RIGHT), 4.07 (DOWN),
and 3.95 (UP) cm away from the source and 5 cm away
from the table plane to minimize the scattered photon
effect on the measurement results.[12] The measurement
points were different from each other due to the
structure of the prepared setup and the source could
not be placed in the midline. A single source position
was set on the applicator and the height of this position was adjusted to be located at the center of the measurement
points. Using the Acuros BV planning algorithm,
a treatment plan was made to obtain a dose of 3 Gy
at the measurement point on the left side containing
the speculum blade. The irradiation duration, obtained
here, was also used in the TG43 planning algorithm
where the same CT image sections were used.
Radiochromic Film (GAFChromic Film) Dosimetry
Calibration and Measurements Made
In the dosimetric measurements made using Radiochromic
film (Ashland Specialty Ingredients, Bridgewater,
NJ, United States of America), first, the calibration
curves of these films were obtained. To this end,
the Varian GammaMed Plus iX model brachytherapy
device (Varian Medical Systems, Palo Alto, United
States of America), located at the Radiation Oncology
Department of the Faculty of Medicine Hospital of
Eskişehir Osmangazi University and contains a 192Ir
radioactive source, was used. For the calibration of the
radiochromic films, the films were cut into a size of
2.5 cm×2.5 cm. The films were cut using scissors and
the films were handled using gloves to avoid any stains
on film surfaces. The cut radiochromic films were categorized into two groups as irradiation and control.
The irradiation group consisted of the films to be irradiated
at the brachytherapy device. The films in the
control group were not irradiated, and they were used
to eliminate the tarnishing resulting from the ambient
radiation in radiochromic films during the time between
irradiation and scanning. Both groups of films
were read in an Epson Expression 11000XL scanner
(Epson Seiko Corporation, Nagano, Japan) to get a
minimum lateral scattering effect before moving to
the irradiation process.[13] To minimize the reading
uncertainty resulting from the scanner, the scanning
surface of the scanner was cleaned before the reading
process, and it was opened 15 min before the scanning
process. After the film readings were completed,
the test apparatus was set up and CT was performed
before being transferred to the TPS. The test apparatus
was set using the approximate water equivalent
solid phantoms (RW3 Slab Phantom, PTW-Freiburg,
Freiburg, Germany) to ensure sufficient backscattering
and the guiding tube with code no. GM11011180
was placed at the center of these phantoms. The TPS
was used to determine dose values at different distances.
A total of 8 dose values were determined and these
dose values were in the range of 1.0 and 6.0 Gy including
the 3-Gy dose value, which is the dose value in the
irradiation to be performed using the speculum. After
these processes, radiochromic films were placed at the
designated distances, and irradiation was performed for the duration calculated using the planning system.
Following the irradiation, the film was kept still for 48
h for the slowdown of polymerization on the film before
the scanning process.[14,15] Both the irradiated
films and the control films that were not irradiated
were scanned approximately 48 h after the irradiation
process. A red channel was used for the scanning. The
mean pixel values of 5 different Regions of Interest of
each film were determined with the Image J software
program (National Institutes of Health, 1997) using
the images obtained. Using the formulas, (a), (b), (c),
(d), and (e) the optical density (OD) values corresponding
to the doses were calculated (Figs. 3, 4).[14]
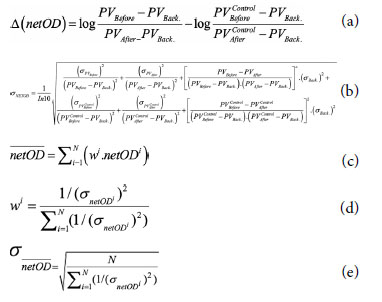
Fig. 3. Control and irradiated GAFChromic films used in GAFChromic dosimetry.
Fig. 4. Measurement of control and irradiated GAFChromic films in GAFChromic dosimetry.
The values obtained were used to draw dose versus OD calibration curves. The calibration curves were later used to measure dose values from the measured OD values of the tarnishing on the film as a result of experimental irradiation.
Following the calibration of radiochromic films, the test apparatus, described above, was used to perform the irradiation of radiochromic films on the brachytherapy device at the sides with and without the speculum.
The speculum blades manufactured from the PEEK material were placed inside the measurement apparatus and their CT images were taken for planning purposes. The CT sections obtained were transferred, and two different brachytherapy applications were prepared using ACUROS BV and TG43 algorithms at the same source position and for the same duration (Figs. 5, 6). In the planning stage, the aim was to create a minimum dose of 3 Gy at the farthest measurement point, and an irradiation duration of 631.1 s was calculated for the single source Dwell position in the planning made using the ACUROS BV algorithm for this purpose. The activity during the irradiation was 11.086 Ci.
Fig. 5. Dose color wash and isodose distributions, ACUROS BV algorithm.
Fig. 6. Dose color wash and isodose distributions, TG43 algorithm.
In the brachytherapy planning made using two different algorithms, the irradiation was performed, and film dosimetry was conducted without changing the test apparatus and ensuring that GAFChromic films were placed to align them with the source. The dose values obtained from the TPSs using two different algorithms and the two different irradiations for the duration obtained from the planning and the mean values of two different assessments for each are given in Figure 7.
Fig. 7. Schematic view of dose values obtained with three different measurement methods.
Statistical Analysis
Categorical variables were described as counts and percentages
(%), whereas continuous variables were described
as means (±standard deviation). The correlations
(r values) were assessed using Pearson's correlation coefficient.
All tests of significance were two-tailed with p<0.01.
Results
The graph showing the dose distribution in four directions obtained using the ACUROS BV algorithm is given in Figure 8, and it is seen that the curves exhibit parallelism in four directions. The graph showing the dose distribution in four directions obtained using the TG43 algorithm is given in Figure 9, and it is seen that the curves exhibit parallelism in four directions. The graph showing the dose distribution directions obtained using the ACUROS BV and TG43 algorithms at the points determined at the level of the Dwell position of the radioactive source and obtained from these points using the GAFChromic dosimetry method is given in Figure 10, and it is seen that the curves exhibit parallelism.Fig. 10. Dose distributions with three different measurement methods.
The correlation of the doses obtained using the ACUROS BV and TG43 algorithms at the points determined at the level of the Dwell position of the radioactive source and obtained from these points using the GAFChromic dosimetry method was performed, and it was found that the values obtained using each of three methods were correlated to each other (p<0.001 for ACUROS BV vs. TG43, p=0.008 for ACUROS BV vs. GAFChromic Film, p=0.006 for TG43 vs. GAFChromic Film) (Table 1).
Table 1 Correlation of dose values obtained from three different measurement methods
Discussion
The purpose of brachytherapy treatment, which is a standard treatment approach in patients diagnosed with locally advanced cervical cancer, is to place radioactive sources near or inside the tumor. OARs such as the rectum or bladder must be protected as the target is exposed to a high dose of irradiation. To this end, different types of applicators are used to keep OARs away from the radioactive source, and vaginal gauze packing is a widely used method.[16] As the vaginal speculum is removed after the placement of the packing, its spoonshaped blades may cause difficulties. This project aimed to modify the vaginal speculum that is currently available in the market and routinely used in daily practice by producing the lower and upper blades of the vaginal speculum using a PEEK material and performing dosimetric measurements and testing the feasibility of the resulting modification for brachytherapy applications.Two different dosimetry methods (TPS and Radiochromic Film Dosimetry System [GAFChromic: EBT3]) were used to perform dosimetry, and it was found that the values calculated using the three methods were correlated to each other. Examination of the dose-distance curves revealed that the modified speculum did not have any adverse contribution to the dose scattering, and it has to be supported by trials to mention that the speculum blades produced from the PEEK material can be used for brachytherapy applications. However, there are different measurement methods in terms of dosimetry, and in this study, film irradiation was performed at two different times to measure the dose obtained from two different planning algorithms, and the measurement of each film was performed twice. In a total of four assessments, different results were obtained. For this reason, mean dosimetric measurements were given in this study. In the literature, an uncertainty of approximately 7% for lower doses and above 8% for higher doses was reported, and lower rates of uncertainty were reported using different dosimetry methods such as Metal Oxide Semiconductor Field Effect Transistor and Optically Stimulated Luminescence.[17-20].
Conclusion
When the dose values obtained from the same points using three methods and the dose scattering belonging to two different planning algorithms were examined, it was found that values exhibited parallelism, and the speculum blades redesigned from scratch with a modular structure and produced from the PEEK material using a 3D printer did not have any negative effect on the dose scattering. However, this proposition should be supported by conducting more measurements using different dosimetry methods.Peer-review: Externally peer-reviewed.
Conflict of Interest: All authors declared no conflict of interest.
Financial Support: This study has been supported by the Eskişehir Osmangazi University Scientific Research Projects Unit with project number TSA-2021-2143.
Authorship contributions: Concept - A.Ö.; Design - A.Ö.; Supervision - A.Ö.; Data collection and/or processing - A.Ö., K.D.; Data analysis and/or interpretation - A.Ö., K.D.; Literature search - A.Ö., K.D.; Writing - A.Ö., K.D.; Critical review - A.Ö., K.D.
References
1) Bailey HH, Chuang LT, duPont NC, Eng C, Foxhall
LE, Merrill JK, et al. American Society of Clinical
Oncology Statement: human papillomavirus
vaccination for cancer prevention. J Clin Oncol
2016;34(15):1803-12.
2) Kamangar F, Dores GM, Anderson WF. Patterns of
cancer incidence, mortality, and prevalence across five
continents: Defining priorities to reduce cancer disparities
in different geographic regions of the world. J
Clin Oncol 2006;24(14):2137-50.
3) Green JA, Kirwan JM, Tierney JF. Survival and recurrence
after concomitant chemotherapy and
radiotherapy for cancer of the uterine cervix:
A systematic review and meta-analysis. Lancet
2001;358(9284):781-6.
4) National Comprehensive Cancer Network. Cervical
Cancer (Version 1.2021). Available at: https://www.
nccn.org/professionals/physician_gls/pdf/cervical.
pdf. Accessed Oct 22, 2020.
5) Lanciano RM, Won M, Coia LR, Hanks GE. Pretreatment
and treatment factors associated with improved
outcome in squamous cell carcinoma of the
uterine cervix: A final report of the 1973 and 1978
patterns of care studies. Int J Radiat Oncol Biol Phys
1991;20(4):667-76.
6) Hanks GE, Herring DF, Kramer S. Patterns of care outcome
studies. Results of the national practice in cancer
of the cervix. Cancer 1983;51(5):959-67.
7) Coia L, Won M, Lanciano R, Marcial VA, Martz K,
Hanks G. The patterns of care outcome study for cancer
of the uterine cervix. Results of the second national
practice survey. Cancer 1990;66(12):2451-6.
8) Montana GS, Martz KL, Hanks GE. Patterns and sites
of failure in cervix cancer treated in the USA in 1978.
Int J Radiat Oncol Biol Phys 1991;20(1):87-93.
9) Logsdon MD, Eifel PJ. Figo IIIB squamous cell carcinoma
of the cervix: An analysis of prognostic factors
emphasizing the balance between the external beam
and intracavitary radiation therapy. Int J Radiat Oncol
Biol Phys 1995;43(4):763-75.
10) Banerjee R, Kamrava M. Brachytherapy in the treatment
of cervical cancer: a review. Int J Womens Health
2014;6:555-64.
11) Li M, Tian F, Jiang J, Zhou M, Chen Q, Zhao D,
Zhai W, et al. Robust and Multifunctional Porous Polyetheretherketone Fiber Fabricated via a Microextrusion
CO2 Foaming. Macromol Rapid Commun.
2021;42(22):e2100463.
12) Nucléide-Lara Library for gamma and alpha emissions,
2021. Available at: http://www.nucleide.org/
Laraweb/index.php. Accessed Feb 21, 2023.
13) Battum VLJ, Huizenga H, Verdaasdonk RM, Heukelom
S. How flatbed scanners upset accurate film dosimetry.
Phys Med Biol 2016;61(2):625-49.
14) Devic S, Tomic N, Lewis D. Reference radiochromic
film dosimetry: Review of technical aspects. Phys Med
2016;32(4):541-56.
15) Duruer K, Etiz D, Yücel H. Investigation of EBT3
radiochromic film response in a high-dose range
of 6 MV photon and 6 MeV electron beams using
a three-color flatbed scanner. East Eur J Phys
2020;3:11-8.
16) Biltekin F, Gultekin M, Yilmaz MT, Yildiz, F. Dosimetric
comparison of two different applicators and rectal
retraction methods used in inverse optimizationbased
intracavitary brachytherapy for cervical cancer.
J Contemp Brachytherapy 2020;12(1):35-43.
17) Oare C, Wilke C, Ehler E, Mathew D, Sterling D, Ferreira
C. Dose calibration of Gafchromic EBT3 film for
Ir-192 brachytherapy source using 3D-printed PLA
and ABS plastics. 3D Print Med 2019;5:3.
18) Carrara M, Romanyukha A, Tenconi C, Mazzeo D, Cerrotta
A, Borroni M, et al. Clinical application of MOSkin
dosimeters to the rectal wall in vivo dosimetry in gynecological
HDR brachytherapy. Phys Med 2017;41:5-12.





